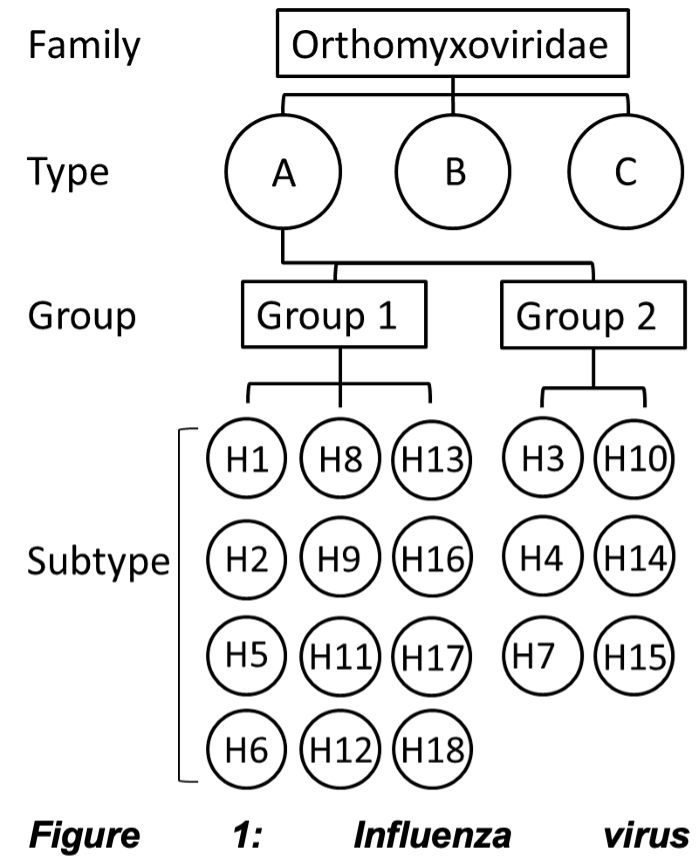
Influenza are negative-stranded RNA viruses belonging to the Orthomyxoviridae family. Influenza circulates in three serotypes (types), of which influenza A virus (IAV) is differentiated into 2 groups and 18 subtypes (Figure 1). IAV subtypes H1N1 and H3N2 and influenza B cause seasonal epidemics. Current influenza vaccine is a mixture of each of these antigens. Due to the high variability and continuous mutations in influenza surface proteins, vaccine antigens must be updated regularly based on prediction of the next likely dominant strains. Mismatch between the predicted vaccine strains and circulating strains can occur, leading to suboptimal efficacy [1]. According to WHO, annual epidemics of influenza gives rise to ~1 billion infections, 3–5 million cases of severe illness, and 300,000–500,000 deaths despite the availability of licensed vaccines [2]. Human infection is caused by respiratory contact with aerosols containing virus particles and it can cause lung inflammation and pneumonia. Four influenza pandemics have occurred since 1900 with the 1918 Spanish flu being the most severe, resulting in >40 million deaths worldwide [3]. Influenza virus is considered Category C Priority Pathogen by the National Institute of Allergy and Infectious Diseases (NIAID).
Relevant bibliography:
[1]Krammer, F.; García-Sastre, A.; Palese, P., Is It Possible to Develop a "Universal" Influenza Virus Vaccine? Potential Target Antigens and Critical Aspects for a Universal Influenza Vaccine. Cold Spring Harb Perspect Biol 2018, 10 (7).
[2]https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
[3]https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html
