Hepatitis C virus (HCV) is a positive-stranded RNA virus belonging to the Flaviviridae family. HCV infection causes inflammation of the liver, that sometimes spontaneously clears within 6 months. However, in the majority of infectied people, the infection becomes chronic. However, the acute infection is often asymptomatic or causes unspecific symptoms. Therefore, HCV infection can remain undetected for decades until the patient develops liver cirrhosis or liver cancer. It is estimated that 1-2% of the world’s population are chronically infected with HCV, and 1.5 million new infections occur annually. Approximately 300,000 people die from hepatitis C infection each year. Direct-acting antiviral (DAA) therapies exist that are able to treat patients with persistent HCV, but treatments are very expensive and unavailable in many parts of the world, such as developing countries.
No vaccine exists to date that protects from HCV infection. One reason is the large genetic diversity of the virus, in particular of the surface-exposed envelope glycoproteins. Therefore, no two hepatitis C virions “look” the same to the immune system and antibodies generally only recognize one isolate of the virus. Vaccine candidates that induce such strain-specific antibodies would not be able to protect from the majority of circulating strains.
In addition, the surface of the virus is covered in carbohydrates which are produced by the human host cells and are recognized as “self” by the immune system. These carbohydrates therefore shield the underlying viral surface from Detection by the immune system.
Despite these countermeasures that the virus uses to evade the immune system, some rare antibodies have been found that are capable of recognizing most or all HCV strains. These so-called “broadly neutralizing” are therefore templates for rational vaccine design.
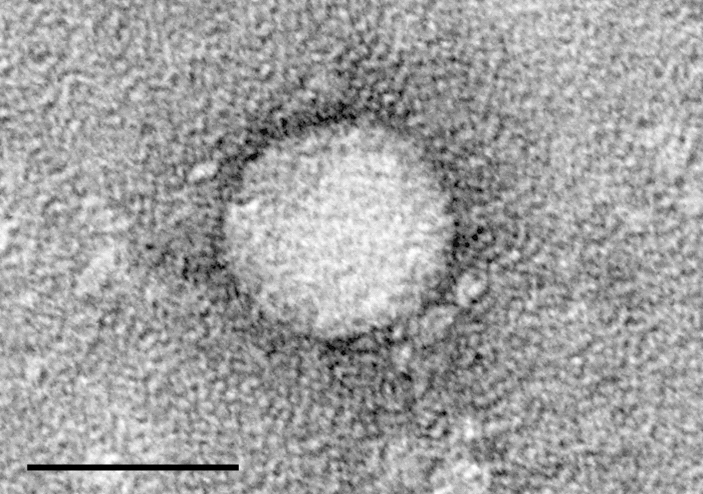
Electron micrograph of a Hepatitis C virion. The bar indicates 50 nm. Downloaded from: https://upload.wikimedia.org/wikipedia/commons/3/3b/HCV_EM_picture_2.png
